Case Report - (2024) Volume 11, Issue 2
A case of incarcerated urethral prolapse requiring surgical intervention in a pediatric patient
Jennifer R Mihalo*, Alaa Al Hajji and Osama Al-OmarAbstract
We present a case of urethral prolapse in prepuberal female that presented with vulvar bleeding. A full medical history from both the patient and her parents in addition to a physical examination by the pedi- atric urology team were done and revealed incarcerated urethral prolapse. Treatments range from medical management to immediate surgical repair; in our case surgical repair was successfully performed. This case report discusses the uncommon manifestations of urethral prolapse in young girls with no previously known risk factors for urethral prolapse.
Keywords
Urethral prolapse, Incarcerated prolapse
Introduction
Urethral prolapse is a rare condition with a low incidence of approximately 1/5000 children that occurs when the proximal part of the urethra descends into the distal part [1]. Patients may present with varying symptoms, most commonly vulvar bleeding, but they may also report pain when wiping or during urination. Treatment depends on the severity of prolapse and ranges from conservative medical treatment (estrogen creams, analgesics, antiseptics) to surgical repair for more severe forms involving incarceration and/or necrosis. Because of its rarity, many cases are misdiagnosed and believed to be secondary to sexual abuse or vaginal trauma. There are a variety of factors that increase the risk of developing urethral prolapse, including urinary tract infection, trauma, constipation, and chronic cough (asthma). Additionally, it appears to be more prevalent in specific ethnicities, such as African American and Hispanic populations [1-5]. Here, we showcase a case of urethral prolapse in a young white girl with no known risk factors.
Case presentation
An 8-year-old white girl presented to the Emergency Department (ED) with vulvar bleeding. The initial examination revealed a bleeding mass protruding from the vulva, prompting consultations for pediatric gynecology and pediatric urology. A comprehensive history was obtained from both the patient and her mother. Her only symptom was painless bleeding on her underwear noticed by her mother. Both the patient and her mother denied recent trauma, urinary symptoms of frequency, urgency, dysuria, or chronic constipation. Her past medical history was unremarkable except for eczema. She had no history of chronic respiratory illnesses or cough but had recently experienced a short upper respiratory tract infection. There was no significant family or surgical history.
Laboratory results were normal, including urinalysis, which was negative for blood, leukocytes, or bacteria. She also underwent pelvic ultrasound which noted the mass to be a homogeneous soft tissue density with internal vascularity as well as noted large stool ball within the rectum. She was also noted to have a large stool ball within the rectum. Renal bladder ultrasound did not identify any anatomical abnormalities or hydronephrosis. Upon physical examination, she was noted to have a bulging mass protruding through the urethral meatus. To confirm the mass’s origin, a catheterization attempt was made with the return of urine. An area of necrosis was noted at the 5-9 o’clock position on the ventral portion of the urethral tissue (Figure 1). The prolapse was unable to be reduced with bedside sedation. Due to concern for incarceration and possible urinary retention, the decision was made to proceed with an examination under anesthesia and possible surgical repair.
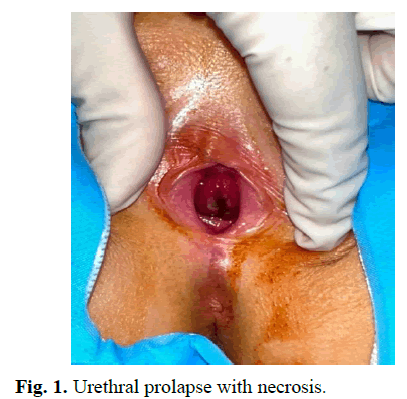
Fig. 1. Urethral prolapse with necrosis.
Further examination under anesthesia revealed friable mucosa and significant edema, as well as a small area of necrosis from 5-9 o’clock on the ventral portion of the urethral tissue. Cystoscopy was performed, which again confirmed urethral prolapse without other intravesical abnormalities. Next, vaginoscopy was performed, revealing an atraumatic cervix and vaginal mucosa without abnormalities or signs of trauma and an intact hymen. The anterior and lateral portions of the prolapsed urethral mucosa were able to be reduced, however, the posterior prolapsed wall was edematous and unable to be reduced with manual manipulation. We then placed a 12 Fr silicone Foley catheter into the urethra excised an ellipsoid portion of necrotic appearing posterior urethral mucosa. Following excision, 4-0 Vicryl suture was utilized in a simple interrupted manner to anastomose the urethral mucosal edges. We then replaced the 12 Fr silicone catheter with a 14 Fr silicone catheter and applied Premarin cream to the incision. There were no immediate post-operative complications (Figure 2). She was discharged home with Premarin cream to use three times a day for 10 days, and instructed to removed her catheter at home in 7 days. She was given acetaminophen and ibuprofen and given oxybutynin and antibiotics for one week while the catheter is in place. She returned to clinic 6 weeks later where her surgical incisions were found to be healed and she had no additional complaints.
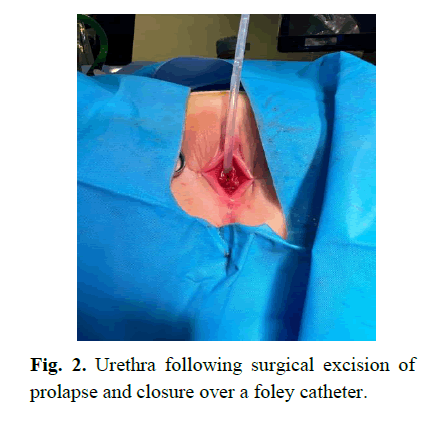
Fig. 2. Urethra following surgical excision of prolapse and closure over a foley catheter.
Results and Discussion
We present a case of symptomatic urethral prolapse requiring surgical intervention in a prepubertal girl without predisposing risk factors which highlights the importance of conducting a detailed medical and social history in additional to focused physical examination. While our patient denied chronic constipation, she did have large stool burden within the rectum which could be a contributing risk factor. Identifying urethral prolapse can be challenging to identify and distinguish from other conditions which could present similarly (vulvar trauma, sarcoma botryoids, ureterocele prolapse, pelvic organ prolapse) [1-4]. This is especially important in more severe cases in which there is necrosis or incarceration requiring prompt diagnosis and surgical treatment.
Urethral prolapse is uncommon in pediatric patients, however certain risk factors can contribute to its development. This condition is associated with weakened pelvic floor muscles resulting from prolonged elevation in intraabdominal pressure. Key risk factors include chronic issues such as constipation, persistent coughing as seen in asthma cases, obesity, urinary tract infections, trauma, and sexual abuse. These factors collectively stand out as the most prevalent contributors to urethral prolapse in the pediatric age group. While the role of genetics in the development of urethral prolapse among children remains unclear, researches indicate a higher prevalence of this condition in the African American and Hispanic populations. However, this can occur without any of these risk factors as demonstrated by the case above indicating that there should continue to be a high degree of suspicion based on symptoms and clinical exam.
There are various modalities for treating urethral prolapse. The most frequently recommended treatment is topical estrogen therapy, sitz baths, and pain/ symptom control. However, persistent and more severe forms of urethral prolapse may require prompt surgical intervention. In particular, in cases where there is noted to be necrosis of the urethra, prompt excision of the lesion is required to prevent further complications such as suprapubic pain, dysuria, hematuria, urinary retention and urethral bleeding. Additionally, persistence of the prolapse should warrant more investigations to rule out urethral polyp as a diagnosis, for that reason an assessment of the lesion and reduction under general anesthesia is sometimes necessary to confirm the diagnosis of urethral prolapse as well as proceed with a surgical repair [6-8].
Conclusion
Despite lack of predisposing factors, we maintained a high index of suspicion based on clinical presentation and initial exam. Cystoscopy and vaginoscopy under anesthesia were performed to confirm the diagnosis of urethral prolapse. Furthermore, we were concerned for possible incarceration and urinary retention so examination under general anesthesia was performed and confirmed the presence of a necrotic area of the urethra which granted the importance of a surgical excision to prevent future complications. This case highlights the importance of conducting a detailed medical history and focused physical examination to reach the correct diagnosis. Urethral prolapse misdiagnosis frequently occurs due to the rarity of such cases, especially in young white girls.
References
- Fiogbe M, Hounnou G, Koura A, et al. Urethral mucosal prolapse in young girls: A report of nine cases in Cotonou. Afr J of Paediatr Surg. 2011;8(1):12-14.
[Crossref] [Google Scholar] [PubMed]
- Fornari A, Gressler M, Murari JCL. Urethral prolapse: A case series and literature review. J Obstet Gynaecol India. 2020;70(2):158-162.
[Crossref] [Google Scholar] [PubMed]
- Wei Y, Wu SD, Lin T, et al. Diagnosis and treatment of urethral prolapse in children: 16 years’ experience with 89 Chinese girls. Arab J Urol. 2017;15(3):248-253.
[Crossref] [Google Scholar] [PubMed]
- Yddoussalah O, Attya AIA, Ettayebi F, et al. Urethral prolapse in young girls: A report of eight cases. J Urol Res. 2018;5(2):1101.
[Crossref]
- Oliyide A, Chibuzo I, Kujawa M. Thrombosed Urethral Prolapse: A case series and review of the literature. J Clin Urol. 2023;16(3).
- Hall ME, Oyesanya T, Cameron AP. Results of surgical excision of urethral prolapse in symptomatic patients. Neurourol Urodyn. 2017;36(8):2049-2055.
[Crossref] [Google Scholar] [PubMed]
- Healey KD, Phrathep DD, Herson AB, et al. Successful surgical management of Urethral prolapse in a postmenopausal female. Cureus. 2023;15(5):e38818.
[Crossref] [Google Scholar] [PubMed]
- Shurtleff BT, Barone JG. Urethral Prolapse: Four quadrant excisional technique. J Pediatr Adolesc Gynecol. 2002;15(4):209-211.
[Crossref] [Google Scholar] [PubMed]
Author Info
Jennifer R Mihalo*, Alaa Al Hajji and Osama Al-OmarReceived: 03-Apr-2024, Manuscript No. PUCR-24-131361; , Pre QC No. PUCR-24-131361; Editor assigned: 05-Apr-2024, Pre QC No. PUCR-24-131361; Reviewed: 19-Apr-2024, QC No. PUCR-24-131361; Revised: 26-Apr-2024, Manuscript No. PUCR-24-131361; Published: 03-May-2024, DOI: 10.14534/j-pucr.20222675636
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
