Case Report - (2021) Volume 8, Issue 6
A rare entity: Median raphe cyst in a boy and review of the literature
Levent Cankorkmaz1*, Ö Fahrettin Göze2, Mehmet H Atalar3 and Gökhan Köylüoğlu4Abstract
Median raphe cysts of the perineum are uncommon congenital lesions of the male genitalia. They can develop at any site along the midline of the ventral side of the genital area, from the meatus to the scrotum and perineum. A 9-year-old patient presented with a cystic nodule in the scrotum just medial mass that at the midline of the scrotum had been present from childhood as long as he could remember. The Magnetic Resonance Imaging (MRI) showed the cyst extended along the midline perineum.There was not communication between the cyst and the urethra. Median raphe cysts in children should be considered in the differential diagnosis of scrotal masses.
Keywords
Median raphe, cyst, child, scrotum
Introduction
Median Raphe Cyst (MRC) of the perineum is an uncommonly encountered clinical condition. These cysts are benign congenital lesions of the male genitalia [1]. It was first described by Mermet [2,3]. These cysts can occur in the midline, following the raphe, from the meatus to the scrotum and perineum [1]. The cyst is generally solitary, with the penile shaft being the most common location, with average size of around 1 cm. Other terms apart from MRC have been used: Mucus cyst of the penis, genitoperineal cyst of the medium raphe, parameatal cyst, hydrocystadenoma, apocrine cystadenoma and urethroid cyst although these cysts are now known referred to as median raphe cysts because they have similar clinical and histologic characteristics[4]. We are presenting a case of a scrotal MRC which presented with symptoms in a boy.
Case Presentation
A 9-year-old boy presented with a soft, nontender cystic nodule lesion of about 2 cm diameter at the scrotum just medial that had been present from childhood as shown in Fig 1. The examination revealed a mass at the midline of the scrotum; the mass was soft, elastic, and non-painful, and did not appear to be adhered to scrotal skin. Rest of the genital examination was normal. Ultrasonographic (USG) examination demonstrated an isoechoic cystic lesion at the scrotal raphe, without any evidence of solid component or septation.

Figure 1: Scrotal median raphe cyst.
The MRI study of the pelvis and perineum showed the morphology, fluid content, and absence of any communication between the mass and other structures or organs (Figs 2A and 2B), the size was 2.5 × 1.5 × 1.5 cm. On T1-weighted images, the cyst was hyperintense depending on the content. There was not communication between the cyst and the urethra. There was not required another radiological examination (eg. voiding and retrograde cystourethrography). On the basis of clinical and radiologic findings, a diagnosis of MRC of scrotal raphe.
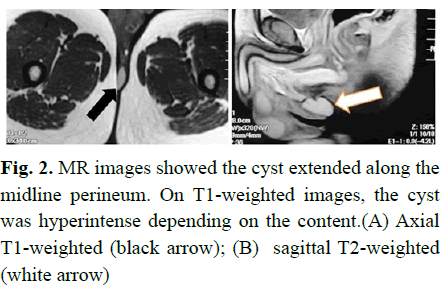
Figure 2: MR images showed the cyst extended along the midline perineum. On T1-weighted images, the cyst was hyperintense depending on the content.(A) Axial T1-weighted (black arrow); (B) sagittal T2-weighted (white arrow)
The cyst was completely excised under general anesthesia. The histological study of the surgical specimen with hematoxylin and eosin staining showed a unilocular cystic cavity, with mucus-fluid content, partially lined by pseudostratified epithelium, PAS (-), D-PAS (-), mucicarmine (-) as well as particularly keratinizing squamous epithelium (Figs 3-5). Histopathological diagnosis was median raphe cyst. The patient was discharged the post-op first day in stable condition. The patient made a good recovery. There was no evidence of recurrence in 5 years of follow-up.
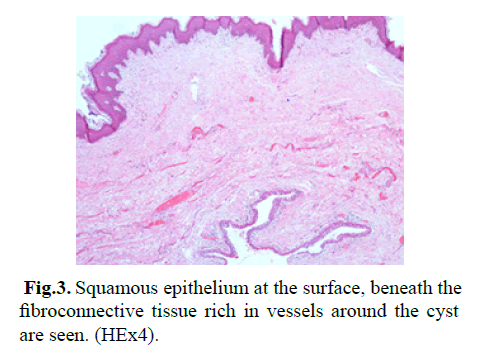
Figure 3: Squamous epithelium at the surface, beneath the fibroconnective tissue rich in vessels around the cyst are seen. (HEx4).
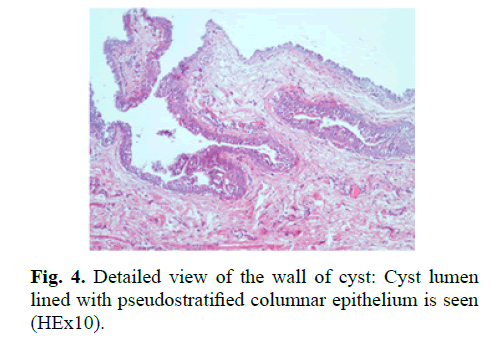
Figure 4: Detailed view of the wall of cyst: Cyst lumen lined with pseudostratified columnar epithelium is seen (HEx10).
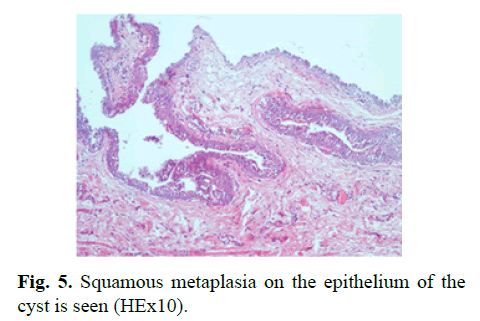
Figure 5: Squamous metaplasia on the epithelium of the cyst is seen (HEx10).
Results and Discussion
MRC is a rare congenital entity. Four histologic patterns have been described:
• Urethral type lined with pseudostratified columnar epithelium (urothelium);
• Epidermoid type, with squamous stratified epithelium;
• Glandular type, lined by urethral epithelium with interspersed glandular structure;
• Mixed type (associated with both epithelial). The urethral type frequency is 70.1% [5,6]. Our cases MRC was urethral type.
The cyst is most commonly noticed in the first decade of life; however, because of the condition being asymptomatic, the patient often presents during second to third decades of life. In our case, the cyst that had been present from childhood as long as he could remember. Two theories have been proposed about the aetiology of MRC. One is the development of embryologic outgrows of epithelium after primary closure of the urethral or genital folds, another is that they arise from epithelial remains caused by incomplete closure of the folds [5]. The cyst is generally solitary, sometimes double, and rarely presents as a chain of cystic swellings along the median raphe [6].
The majority of the cysts do not reach size in excess of 1 cm [6]. Scrotal cysts tend to be larger than cysts elsewhere [6]. In our patient, the size of the cyst was about 2.5 cm, which made it larger than the mean observed size of these cysts. MRCs with sizes in excess of 2 cm have also been reported [6].
The diagnosis is mostly clinical, radiological imaging have a limited role. USG shows an isoechoic cystic lesion in our patient.USG can help to rule out vascularity [6]. Like USG, MRI also helps in determining the anatomical extent of the cyst [4,6].
MRC may be secondarily infected and manifest as pain, tenderness, erythema, or pus discharge. Infection of the cyst is generally a phenomenon after sexual activity. Nevertheless the cyst may also be traumatized by other means and become infected [6].
Treatment should be considered for the symptomatic lesions and for cosmetic purposes. The treatment options include a wide local excision and aspiration. Aspiration is not recommended for the MRC’s, because of aspiration may be associated with recurrence [7]. Marsupialisation or deroofing are performed in the cases of deeply located great cysts, which are cosmetically unsatisfactory, and these procedures should be avoided [8]. Usually, no surgical complications are reported [7]. Hence, a complete excision is the preferred treatment of choice.
Conclusion
MRC in children should be considered in the differential diagnosis of scrotal masses. The lesions are congenital and readily diagnosed clinically, but usually diagnosed in adulthood rather than childhood because they are often not evident for years and typically silent. MRI could be used for the differential diagnosis of scrotal cysts in children (as well as without radiation).
References
- Nagore E, Sánchez‐Motilla JM, Febrer MI, et al. Median raphe cysts of the penis: A report of five cases. Pediatr Dermatol. 1998; 15:191-3.
- Memert P. Congenital cysts of the genitoperineal raphe. Rev Chir. 1895; 15:382-435.
- Dini M, Baroni G, Colafranceschi M. Median raphe cyst of the penis: A report of two cases with immunohistochemical investigation. Am J Dermatopathol. 2001; 23:320-4.
- Navarro HP, Lopez PC, Ruiz JM, et al. Median raphe cyst: Report of two cases and literature review. Arch Esp Urol. 2009; 62:585-9.
- Krauel L, Tarrado X, Garcia-Aparicio L. Median raphe cysts of the perineum in children. Urology. 2008; 71:830-1.
- Syed MA, Amatya B, Sitaula S. Median raphe cyst of the penis: A case report and review of the literature. J Med Case Rep. 2019; 13:1-9.
- Shao IH, Chen TD, Shao HT, et al. Male median raphe cysts: Serial retrospective analysis and histopathological classification. Diagn Pathol. 2012; 7:1-5.
- Shiraki IW. Parameatal cysts of the glans penis: A report of 9 cases. J Urol. 1975; 114:544-8.
Author Info
Levent Cankorkmaz1*, Ö Fahrettin Göze2, Mehmet H Atalar3 and Gökhan Köylüoğlu42Department of Pathology, Sivas Cumhuriyet University, Sivas, Turkey
3Department of Radiology, Sivas Cumhuriyet University, Sivas, Turkey
4Department of Pediatric Surgery, Katip Çelebi University, İzmir, Turkey
Received: 28-Oct-2021 Accepted: 11-Nov-2021 Published: 18-Nov-2021, DOI: 10.14534/j-pucr.2022.281
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
