Case Report - (2024) Volume 11, Issue 2
A rare giant glans hemangioma in a child: A particulary challenging case
Essamoud S1*, Lahlou M1, Andolfi C2, Klipfel C2, Jochault-Ritz S2, Zerhouni H1 and Geiss S2Abstract
A rare giant glans hemangioma is an uncommon vascular anomaly that occurs in children, characterized by the abnormal proliferation of blood vessels within the glans penis, the sensitive tip of the male genita- lia. While hemangiomas are more commonly found on the skin, having one on the glans is exceptionally rare. These growths typically appear as red or purple nodules, causing swelling and potential discomfort. They can be present at birth or develop shortly after. The exact cause remains unclear, but it’s believed to involve abnormal blood vessel development during fetal development.
Keywords
Glans hemangioma, child, genital hemangioma, surgery
Introduction
According Hemangiomas are the most common benign vascular tumors in pediatric population. However, their genitourinary localization is rare. They are exceptionally described in the genitals. They are the result of the proliferation of immature capillary vessels [1]. Only a few cases of glans hemangioma have been described in the literature. Plenty of ways of treatment has been described such as cryotherapy, lasers and surgery [2,3]. Long-term follow-up may be necessary to monitor for potential complications and ensure the child’s continued growth and development. We present a rare case of a glans lobular hemangioma in a male child discovered after circumcision.
Case presentation
Parents of a 7-year-old male child consulted our clinic for a painless lesion on the glans penis discovered 4 years earlier after circumcision. His past medical and family histories were unremarkable. The lesion seems to have been small at first at the discovery and is slowly growing overtime. On physical examination, it was a 15 mm, strawberry like, compressible lesion on the ventrolateral part of the glans penis. Due to the patient’s age, the glans itself was approximately 30 mm in diameter, making it a giant lesion comparatively (Figure 1).
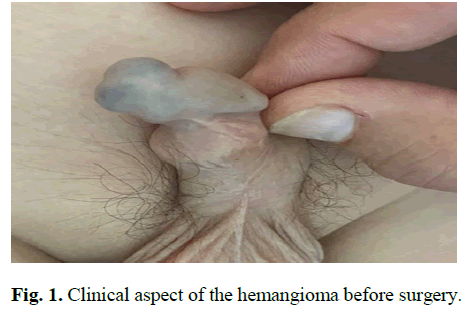
Fig. 1. Clinical aspect of the hemangioma before surgery.
Management was challenging due to its size and site which was in contact to the urethral meatus. Therefore, no conservative treatment options were possible such as cryotherapy, sclerotherapy, nor laser treatments. To confirm that the urethra wasn’t invaded by the tumor, an MRI was performed. It showed a cleavage plan between the lesion and the urethra. No Doppler echography was performed.
Surgical treatment was preferred in this case under general anesthesia. After a Foley catheterization, and without emptying the hemangioma, a tourniquet was applied at the base of the penis. Incision begun far from the urethra, following circumference of the lesion. The mass was carefully dissected. Bleeding was controlled by a bipolar electrocautery. Separation from urethral wall was possible without incident. The entire tumor was removed. Closure of the cutaneal gap was successfully performed by separated stitches with a 6-0 polydioxanone monofilament without tension (Figure 2).
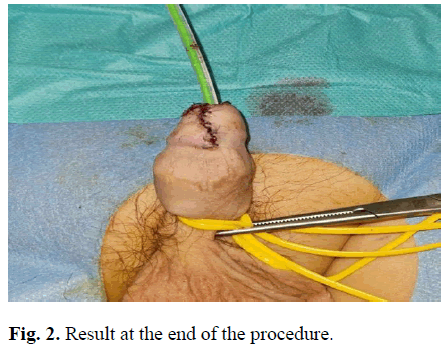
Fig. 2. Result at the end of the procedure.
The postoperative period was unremarkable. The patient was discharged after 48 hours following the procedure during which the Foley catheter was kept. The patient needed non-opioid analgesics and topical Nitrofurazone cream was applied for 7 days. The wound healed completely after 15 days. Follow-up at 2 months showed no recurrence nor scar formation (Figure 3).

Fig. 3. Result at 2 month follow-up.
Results and Discussion
Despite being the most common benign vascular tumors, hemangiomas are rarely localized on the genitals [1]. In a comprehensive review, Dehner and Smith described 10 benign angiomatous lesions of the glans penis [4]. Since then, a few of such lesion has been reported in the literature, and fewer in pediatric populations [2,3,5–8]. Circumstances of discovery may differ. They can be seen right after birth, or after a prepuce-related event. One case of a paraphimosis caused by a hemangioma was described in a 1-year-old boy [6]. In our case, it was discovered after circumcision. Even though it was performed by a physician in another hospital structure, no further management was undertaken. That could be explained by the probably insignificant size of the hemangioma at the time of the procedure. However, long-term follow-up was necessary.
Hemangiomas’ removal is not always necessary. They can remain asymptomatic or cause symptoms [9]. Removal may be necessary if functional symptoms or discomfort are present, or in case of aesthetic issues. In our situation, the lesion was close to the urethral meatus and its size was consequent in comparison to the glans itself. Our fear was that, because of the rate of its growth, it may be more difficult to remove if no treatment was performed. The second one was that it may be an obstacle for vaginal penetration during future intercourses in adulthood. The decision of excision was irrevocable.
In the literature, treatment options are diverse. Less invasive procedures are represented by sclerotherapy and laser treatment. The first one is performed by injecting sclerosing agents such as 30% hypertonic saline or Polidocanol or sodium tetradecyl sulfate into the lesion. It’s a cost-effective technique and is mostly preferred in developing countries [10-12]. It can be done for large hemangiomas but is associated to complications such as risk of cutaneous necrosis, ulceration, and hyperpigmentation [12].
Neodymium:Yttrium-Aluminum-Garnet (Nd:YAG) laser is an excellent method of treatment that provides excellent tissue coagulation without fibrosis and has proven its efficacy in adult cases with good cosmetic results [11], but tissue penetration rate is too deep for small lesions like for instance in pediatric population. Nd:YAG laser has a wavelength of 1060 nm, and when passing through a potassium thiophosphate crystal, it produces a wavelenght of 532 nm, which induces less scatter and less necrotic damage to the surrounding tissue. Harmlessness is the reason Potassium Thiophosphate laser is preferred in children cases [2].
Surgical removal remains the classical therapeutic approach and is an effective treatment option for hemangiomas [3]. It was our preferred solution due to the lesion size and location to the external urethral orifice. Luckily, preoperative MRI showed a cleavage plan with the wall of the urethra and guided our procedure. During the intervention, careful dissection and bleeding control by bipolar electrocautery or similar are obligatory [12]. Injury to the urethra must be avoided as possible. If no other option is feasible, urethroplasty reconstruction must be undergone with cutaneal grafting if necessary [2]. Removal has to be as complete as possible to prevent recurrences [8]. Hemorrhage is the principal risk when removing a hemangioma, especially in concealed locations [2], but it can be minimized by applying a tourniquet at the base of the penis and by using careful cauterization.
Conclusion
Hemangiomas on the glans penis are rare and can be discovered in prepuce-related events. Various treatment options are available and the non-invasive ones are effective with excellent cosmetic results even in pediatric population. Surgical treatment remains a classical approach when no other option is feasible nor available, and s till has great results if performed properly.
References
- Ulker V, Esen T. Hemangioma of the glans penis treated with Nd:YAG laser. Int Urol Nephrol. 2005; 37(1):95–96.
[Crossref] [Google Scholar] [PubMed]
- Kennedy WA, Hensle TW, Giella J, et al. Potassium thiophosphate laser treatment of genitourinary hemangioma in the pediatric population. J Urol. 1993; 150(1):950–952.
[Crossref] [Google Scholar] [PubMed]
- Jimenez-Cruz JF, Osca JM. Laser treatment of gians penis hemangioma. Eur Urol. 1993; 24(1):81–83.
[Crossref] [Google Scholar] [PubMed]
- Dehner LP, Smith BH. Soft tissue tumors of the penis: A clinicopathologic study of 46 cases. Cancer. 1970; 25(1):1431–1447.
[Crossref] [Google Scholar] [PubMed]
- Papali AC, Alpert SA, Edmorson JD, et al. A review of pediatric glans malformations: A handy clinical reference. J Urol. 2008;180(1):1737–1742.
[Crossref] [Google Scholar] [PubMed]
- Yiğiter M, Arda İS, Hiçsönmez A. An unusual cause of paraphimosis: Hemangioma of the glans penis. J Pediatr Surg. 2008; 43(1):31–33.
[Crossref] [Google Scholar] [PubMed]
- Senoh K, Miyazaki T, Kikuchi I, et al. Angiomatous lesions of glans penis. Urology. 1981; 17(1):194–195.
[Crossref] [Google Scholar] [PubMed]
- Akyol I, Jayanthi VR, Luquette MH. Verrucous hemangioma of the glans penis. Urology. 2008; 72(1):15-16.
[Crossref] [Google Scholar] [PubMed]
- Mondal S, Biswal D, Pal D. Cavernous hemangioma of the glans penis. Urol Ann. 2015; 7(1):399-401.
[Crossref] [Google Scholar] [PubMed]
- Hemal AK, Aron M, Wadhwa SN. Intralesional sclerotherapy in the management of hemangiomas of the glans penis. J Urol. 1998; 159(2):415–417.
[Crossref] [Google Scholar] [PubMed]
- Kumar A, Goyal NK, Trivedi S, et al. Primary cavernous hemangioma of the glans penis: Rare case report with a review of the literature. Aesth Plast Surg. 2008; 32(2):386–388.
[Crossref] [Google Scholar] [PubMed]
- Kim KS, Lee H, Hwang JH, et al. Incidentally detected cavernous hemangioma of the glans penis after circumcision: A case report. Medicine. 2020; 99(21):e20217.
[Crossref] [Google Scholar] [PubMed]
Author Info
Essamoud S1*, Lahlou M1, Andolfi C2, Klipfel C2, Jochault-Ritz S2, Zerhouni H1 and Geiss S22Department of Pediatric Surgery, Louis Pasteur II Hospital, Colmar, France
Received: 27-Sep-2023, Manuscript No. PUCR-23-115057; , Pre QC No. PUCR-23-115057; Editor assigned: 02-Oct-2023, Pre QC No. PUCR-23-115057; Reviewed: 16-Oct-2023, QC No. PUCR-23-115057; Revised: 23-Oct-2023, Manuscript No. PUCR-23-115057; Published: 30-Oct-2023, DOI: 10.14534/j-pucr.20222675598
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
