Case Report - (2022) Volume 9, Issue 1
Aphallia: An extremely rare case report
Muhammad Akram Malik1*, Muhammad Waqas Iqbal1, Suaiba Saif2, Adeen Akram3, Asad Ramzan4 and Nauman Khalid1Abstract
Aphallia or penile agenesis is a congenital malformation. This is extremely rare anomaly of urogenital system posing serious medical and psychological problems. Its estimated prevalence is 1 out of 10-30 million births. We hereby present a case of aphalia in a child of 09 years old, who was brought to emergency department with uraemia and urosepsis. Bilateral Percutaneus Nehrostomies (PCN) was performed for marked pyonephrosis. Appendico-vesicostomy (metroffnof) and closure of vesicorectal communication was planned as definitive procedure. Parents of the child refused further surgical procedures and left hospital with no follow up.
Keywords
Aphallia, development of phallus, associated anomalies
Introduction
Aphallia or complete penile agenesis is an extremely rare congenital anomaly with serious medical and psychological issues [1]. Its prevalence is one per 10- 30 million births. Since it was originally described by Imminger in 1853, approximately 100 cases have been described worldwide [2]. Absence or failure in the development of genital tubercle is the main etilogy. Aphallia can be classified in two major groups. First one is the solitary malformation of aphallia. Second one is the complex form which is often incompatible with life because of accompanying congenital anomalies. This syndrome is mesodermal disorder reported with several anomalies including anal stenosis or closed anus, renal dysplasia, lung agenesis, phallus tetralogy, multi spinal disorders like sacrum agenesis, rib segmental and CNS disorders. Kidney agenesis or cystic kidney, horseshoe kidney, vesico-ureteric reflux, prostate agenesis, skeletal and neural disorders, annular pancreas, clubfoot or cardiac abnormalities are usually associated with it [3,4].
As the digestive system and urinary tract caudal embryonic origin are of cloaca segment, vesico rectal or urethro-rectal fistula is seen in these patients. Due to suffering from several disorders, many patients die in a few days after birth. The majority of such patients have 46XY Karyotype. Because of absence of phallus despite male genotype, many of these people suffer from various psychological ailments. Very few cases of patients having aphallia with this age has been reported in the literature. We hereby report an exceptionally rare case of Aphallia along with a review of literature. An informed consent was obtained from parents of this child for case reporting.
Case Presentation
A 0-9 years old was brought to our hospital in emergency department, by his parents with the complaints of fever, vomiting and loss of appetite. He was drowsy with tachycardia and tachypnia. Detailed history revealed an absence of penis since birth and urine being passed through rectum mixed with faecal matter. He was registered as a boy having 46XY chromosomes at his birth. Physical examination revealed total absence of the penis with no urethral opening. Testes were palpable bilaterally with well developed scrotum (Fig 1).The anal opening was located normally.
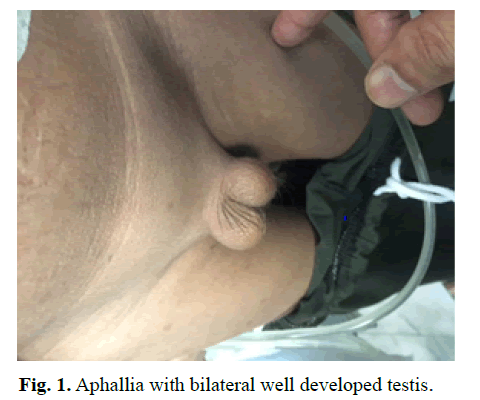
Figure 1: Aphallia with bilateral well developed testis.
On ultrasonography of abdomen and pelvis, severe bilateral hydronephrosis was detected containing infected urine. His RFTs were deranged and CBC showed increased WBCs. No other cardiac and neurological congenital abnormality was found on his detailed clinical examination and investigations. Bilateral PCN was performed under local anesthesia. Infected urine came out which was sent for culture and sensitivity. Broad spectrum antibiotics were started. Patients improved clinically in 3-4 days with normalization of WBC and RFTs.
Antegrade pyelography was performed which showed dilated ureters entering into the bladder and urine leaking into rectum (Fig 2). MRI was performed to assess bladder capacity, its communication with rectum and associated any other congenital anomalies (Fig 3).Counselling of parents for definitive procedures like Appendico-vesicostomy (metroffnof)/permanent vesicostomy and closure of vesicorectal communication was discussed. However Parents of the child refused further surgical procedures and left hospital with no follow up.
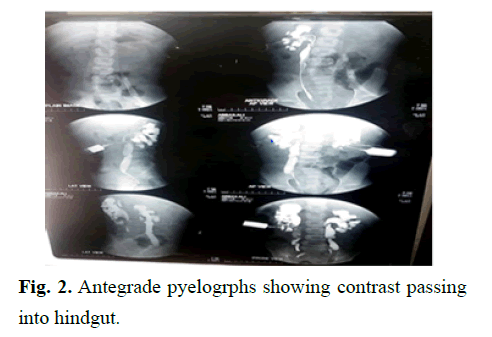
Figure 2: Antegrade pyelogrphs showing contrast passing into hindgut.
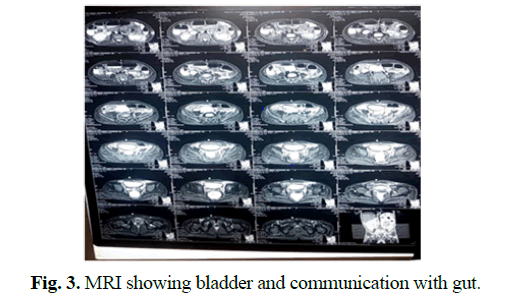
Figure 3: MRI showing bladder and communication with gut.
Results and Discussion
Aphallia or agenesis of phallus is a very congenital disorder. Fewer than 100 cases have been reported worldwide [1-5].This anomaly occurs within 4 weeks of embryonic development. Absent genital tubercle or its developmental impairment is the main etiology. Aphallia has been reported among diabetic mothers. But urogenital system abnormalities are more prevalent among controlled diabetic mothers. In the majority of patients suffering Aphallia, renal agenesis and urinary tract bring about fatal oligohydraminos and subsequently, pulmonary hyperplasia. There may be associated other congenital abnormalities. Due to these reasons there there are higher chances of intrauterine death of child. Even if child is born, he usually dies in early infancy due to these multiple congenital anomalies [6,7]. In our case this child has grown up to the age of 0-9 years. He was having no other associated congenital anomaly and this is the main reason of his survival.
Gerard-Blanluet reported a case of Aphallia with several mesodermal impairments. This newborn had closed anus, dysplastic kidneys, right lung agenesis and rib disorder [6]. In 1999, Gripp reported a case of Aphallia with anal stenosis, phallus tetralogy, and multiple spinal disorders [8]. Patient with Aphallia usually have Karyotype XY46. SRY gene is the sex determining transcription factor on Y chromosome. This gene expression leads to gonadal development of male and internal and external genital system of male gender [9].
Urine usually passes through rectum in these patients. This is usually associated with vesicoureteral reflux and ante-posed anus. Many patients die in a few days after birth due to other associated congenital disorders.If the patients survive in initial months, genital reconstruction and separation of urinary system from rectum are the goals of management. In the past, transgender to female was more preferred approach, due to easiness of vaginoplasty as compared to phalloplasty. However efforts have been made to reconstruct phallus [10]. If the child is going to stay boy as his parents decide, phalloplasty has to be conducted at puberty time. Thanks to IVF advances, having a child will be possible for these patients. Overall, based on novel treatment measures, if the kidney failure is due to its obstruction, these patients will be born in more favorable conditions and future treatment measures will be directed to keep external genitals (male) through timely diagnosis and prenatal surgery and timely bladder drainage (fetal surgery).
In our case keeping our cultural tradition and barriers, transgender surgery may not be preffred choice of the patient and parents. In our case parents of child wanted to grow him as male. We have counselled the parents and child about our suggested management paln by separation of his urinary system from rectum by urinary diversion through permant vesicostomy, appendicovesicostomy or ileal conduit while closing the vesicorectal communication. We have also discussed about the phaloplasty at puberty and chances of having offsprings by assisted reproductive techniques. However when RFTs and general condition of patient improved, his parents left Hospital and did not turn up in follow up.
Conclusion
Aphallia has physical and psychosocial issues. Literature review revealed that if renal failure is due to its obstruction, and there are no associated congenital anomalies, patients may be born in more favorable conditions. Future management will be timely bladder drainage and definitive management at later stage.
Disclosure
We declare that the authors have obtained informed consent from the patient to report this case.
Conflict of Interest
There is no conflict of interest.
Financial Disclosure
The authors declares that this study has received no financial support.
References
- Kane AD, Ngom G, Ndour O, et al. Aphallia: A case report and literature review. Afr J Paediatr Surg. 2011; 8:324.
[CrossRef] [Google Scholar] [Pubmed]
- Wang H, Guo K, Wang J, et al. Aphallia in an adult male with 46, XY karyotype. Int J Urol. 2011; 18:540-2.
[CrossRef] [Google Scholar] [Pubmed]
- Rattan KN, Kajal P, Pathak M, et al. Aphallia: Experience with 3 cases. J Pediatr Surg. 2010; 45:e13-6.
[CrossRef] [Google Scholar] [Pubmed]
- Gredler ML, Seifert AW, Cohn MJ. Morphogenesis and patterning of the phallus and cloaca in the american alligator, alligator mississippiensis. Sex Dev. 2015; 9:53-67.
[CrossRef] [Google Scholar] [Pubmed]
- Willihnganz-Lawson KH, Malaeb BS, Shukla AR. De castro technique used to create neophallus: A case of aphallia. Urology. 2012; 79:1149-51.
[CrossRef] [Google Scholar] [Pubmed]
- Gérard-Blanluet M, Lambert V, Khung-Savatovsky S, et al. Aphallia, lung agenesis and multiple defects of blastogenesis. Fetal Pediatr Pathol. 2011; 30:22-6.
[CrossRef] [Google Scholar] [Pubmed]
- O'Connor TA, Lacour ML, Friedlander ER, et al. Penile agenesis associated with urethral and bilateral renal agenesis. Urology. 1993; 41:564-5.
- Gripp KW, Barr Jr M, Anadiotis G, et al. Aphallia as part of urorectal septum malformation sequence in an infant of a diabetic mother. Am J Med Genet. 1999; 82:363-7.
[CrossRef] [Google Scholar] [Pubmed]
- Goyal A, Bianchi A. The parascrotal flap phallo-urethroplasty for aphallia reconstruction in childhood: Report of a new technique. J Pediatr Urol. 2014; 10:769-72.
- Bajpai M. Scrotal phalloplasty: A novel surgical technique for aphallia during infancy and childhood by pre-anal anterior coronal approach. J Indian Assoc Pediatr Surg. 2012; 17:162.
[CrossRef] [Google Scholar] [Pubmed]
Author Info
Muhammad Akram Malik1*, Muhammad Waqas Iqbal1, Suaiba Saif2, Adeen Akram3, Asad Ramzan4 and Nauman Khalid12Department of Urology, Madina Teaching Hospital, Faisalabad, Pakistan
3DHQ Hospital, Faisalabad, Pakistan
4Department of Urology, Shalamar Medical College, Lahore, Pakistan
Received: 24-Feb-2022, Manuscript No. PUCR-22-52546; , Pre QC No. PUCR-22-52546 (PQ); Editor assigned: 28-Feb-2022, Pre QC No. PUCR-22-52546 (PQ); Reviewed: 10-Mar-2022, QC No. PUCR-22-52546; Revised: 14-Mar-2022, Manuscript No. PUCR-22-52546 (R); Published: 21-Mar-2022, DOI: 10.14534/j-pucr.2022.287
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
