Case Report - (2021) Volume 8, Issue 5
Doppler signs of extravaginal testicular torsion mimicked by small vessel intra-testicular vasculitis in henoch-schoenlein purpura: A case report
Vahid Khajehreza-Shahri1, Sara Gifani2, Paria Dehghanian3, Reza Nazarzadeh4, Ali Mohammad Pourbagher-Shahri5 and Seyed Ali Alamdaran6*Abstract
Henoch-Schoenlein Purpura (HSP) is one of the most common types of multi-systemic vasculitis seen in childhood with “classic triad” of purpura, arthritis, and abdominal pain. Scrotal disease including scrotal swelling, epididymitis, and orchitis are very rare complications of HSP that can mimic the symptoms and signs of testicular torsion, which is one of the major surgical emergencies in children. Radiological modalities are commonly used to diagnose possible causes of acute scrotum such as testicular torsion.
Here we report an 8-year-old boy, complaining of acute pain and swelling in his left testicle. Although colour Doppler ultrasonography of his testes showed increased-size parenchymal echo in the left testicle and its epididymis, with no detectable blood flow on the same side, immediate surgical exploration indicated normal pulse in both testicles’ arteries, with no signs of torsion. Finally, the pathological specimen results were consistent with the diagnosis of HSP-related testicular involvement.
In conclusion, the occurrence of small vessel intra-testicular vasculitis in Henoch-Schoenlein Purpura can mimic clinical and Doppler ultrasonic signs of extravaginal testicular torsion.
Keywords
Henoch-schoenlein purpura, spermatic cord torsion, vasculitis
Introduction
Henoch-Schoenlein Purpura (HSP) is one of the most common types of multi-systemic vasculitis seen in childhood and is characterized by non-thrombocytopenic non-blanching purpura, arthritis, abdominal pain, and renal involvement [1]. However, due to the variety of presenting symptoms and differential diagnoses, HSP diagnosis is not definite in many cases.
Although many antigens, such as food, infective agents, drugs, vaccinations, and insect bites have been reported to be related to HSP, the underlying etiology of this disease is still unclear [2].
Uncommon manifestations of HSP include scrotal disease, pulmonary disease, carditis, and CNS involvement [3]. Scrotal swelling, epididymitis, and orchitis are rarely seen as a complication of this disease [3]. Radiological modalities are commonly used for differential diagnosis of HSP complications and further follow-ups [4].
Here we present and discuss a rare case of HSP, whose color Doppler ultrasonography findings resemble testicular torsion even after a negative exploratory surgery.
Case Presentation
An eight-year-old boy was admitted to our hospital with acute pain and swelling in the left testicle. His medical history was remarkable for a prior admission one week earlier, with bilateral pain and swelling of his ankles followed by palpable purpuric/petechial rash on the extremities. Based on the clinical presentation, and his laboratory and imaging tests results, he had been diagnosed with Henoch-Schoenlein Purpura, and discharged afterwards. His other medical and family histories were unremarkable.
At the time of second admission, patient was not in distress and his vital signs were within the normal range. There was no history of nausea, vomiting, abdominal pain, and trauma to testis. On physical examination, abdomen and chest were normal. Genital exam showed an erythematous and edematous scrotal wall accompanied by enlarged left testicle with mild tenderness and a normal position. The right testicle had a normal size and was non-tender.
On laboratory tests, urine analysis and culture were non-significant. Abnormal findings of the Complete Blood Count (CBC) included Mean corpuscular hemoconcentration, 38.7 (30-36 gm/dl); Platelets, 520 k/uL; Alkaline Phosphatase, 375 IU/L; and ESR, 34 mm/hr.
Color Doppler ultrasonography of testes showed an increase in the size of parenchymal echo in the left testicle and its epididymis with mild heterogeneity. Blood flow was not detected within the left testicle and its epididymis, and moderate peri-testicular hyperemia was present. There were no signs of hydrocele, and the axes of testis were normal (Fig 1).
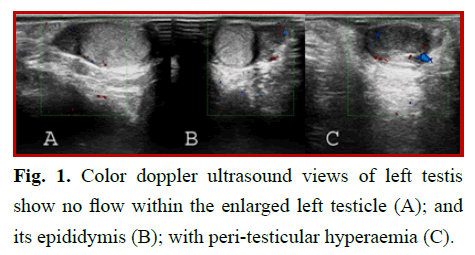
Figure 1: Color doppler ultrasound views of left testis show no flow within the enlarged left testicle (A); and its epididymis (B); with peri-testicular hyperaemia (C).
Although rare in post-neonatal age, extravaginal testicular torsion was suspected and surgical exploration was performed immediately to rule out testicular torsion. Surgery revealed normal pulse in both testicles’ arteries as well as left-sided hemorrhagic epididymis, bruised testis, and no signs of torsion (Fig 2A). A biopsy was also taken and orchiopexy was performed. The pathology report showed diffuse interstitial hemorrhage, leukocytoclastic vasculitis, and small intra-testicular vasculitis with endothelial fibrinoid necrosis of capillaries (Fig 2B).
Figure 2: Macroscopic and microscopic findings of left testicle demonstrate hemorrhagic epididymis and bruised testis without signs of torsion (A); and diffuse interstitial hemorrhage, leukocytoclastic small vessel intra-testicular vasculitis, and small capillaries with fibrinoid necrosis of endothelium (B).
The patient received medical treatment and repeated color Doppler ultrasonography showed an increase in testicular heterogenicity and enhancement of vascularity in peri-testicular soft tissue and periphery of the left testicle. He was discharged the day after with medical treatment.
Discussion
One of the significant surgical emergencies in children is acute scrotum, most common causes of which include testicular torsion, torsion of testicular appendices, orchiepididymitis and scrotal trauma [5]. Hydrocele, idiopathic scrotal edema, and HSP are among the least common causes [5]. In HSP patients, urological manifestations can include kidney involvement, nephritis, obstruction of the ureter, and urethritis [3]. Scrotal involvement in HSP usually results in pain, tenderness, swelling, or discoloration of the scrotum which can be caused by scrotal swelling (the most common), epididymitis, spermatic cord vasculitis, and orchitis [3].
In HSP, scrotal pain can sometimes mimic testicular torsion to various degrees. An accurate medical history, careful physical examination along with appropriate imaging studies are necessary to diagnose painful scrotal swelling associated with HSP [3]. When an acute scrotum is suspected, immediate surgery must be done to save the affected gonad. However, performing imaging tests such as ultrasonography in cases with HSP and testicular pain is necessary to be able to recognize the primary cause and necessary actions required [5].
In color Doppler ultrasonography of patients with testicular torsion, vascular signals in the affected testis are decreased or absent, and evidence of hyperemia surrounding the ischemic or infarcted testicle may be present [5]. Unlike testicular torsion, HSP exhibits normal or increased vascular flow [6,7].
A number of HSP cases with scrotal and testicular involvement have been reported as yet [8-10]. Although spermatic cord vasculitis associated with testicular infarction has been reported in the literature [7], testicular infarction due to vessel involvement is rare [11,12].
As in the present case, lack of blood flow in the affected testis demonstrates that acute scrotum in HSP can mimic testicular torsion and should be considered in the future similar situations as it may require invasive interventions in the course of treatment.
Conclusion
The occurrence of small vessel intra-testicular vasculitis in Schoenlein-Henoch Purpura can mimic clinical and Doppler ultrasonic signs of extravaginal testicular torsion. Despite the fact that HSP is uncommon in adolescence, non-thrombocytopenic palpable purpura involving many organs (gastrointestinal, renal, and joints) should be examined. As seen in this Case Report, prompt diagnosis and multidisciplinary action can lead to proper care and reduce potential complications.
Compliance with ethical statements
Conflicts of interest: None.
Financial disclosure: None.
Consent
Patient confidentiality has been maintained and written informed consent was obtained from the patient’s parent and can be provided as required.
References
- Trnka P. H enoch–S chönlein purpura in children. J Paediatr Child Health. 2013; 49:995-1003.
- Hetland LE, Susrud KS, Lindahl KH, et al. Henoch-schonlein purpura: A literature review. Acta Derm Venereol. 2017; 97:1160-1166.
- Brodie A, Natasha G, Nitiahpapand R, et al. Unusual presentation of henöch-schonlein purpura. Case Reports. 2018.
- Crisci V, Esposito C, Giurin I, et al. Idiopathic scrotal hematoma simulating a testicular torsion, in association with cryptorchidism: US findings. Pol J Radiol. 2014; 79:219-221.
- Ta A, D’Arcy FT, Hoag N, et al. Testicular torsion and the acute scrotum: Current emergency management. Eur J Emerg Med. 2016; 23:160-5.
- Bombiński P, Warchoł S, Brzewski M, et al. Ultrasonography of extravaginal testicular torsion in neonates. Pol J Radiol. 2016; 81:469-472.
- Dalpiaz A, Schwamb R, Miao Y, et al. Urological manifestations of henoch-schonlein purpura: A review. Curr Urol. 2014; 8:66-73.
- Akgun C. A case of scrotal swelling mimicking testicular torsion preceding henoch-schönlein vasculitis. Bratisl Lek Listy. 2012; 113:382-3.
- Modi S, Mohan M, Jennings A. Acute scrotal swelling in henoch-schonlein purpura: Case report and review of the literature. Urol Case Rep. 2016; 6:9-11.
- Dayanır Y, Akdilli A, Karaman C, et al. Epididymoorchitis mimicking testicular torsion in henoch-schönlein purpura. Eur Radiol. 2001; 11:2267-9.
- Fukuda S, Takahashi T, Kumori K, et al. Idiopathic testicular infarction in a boy initially suspected to have acute epididymo-orchitis associated with mycoplasma infection and henoch–schönlein purpura. J Pediatr Urol. 2009; 5:68-71.
- Zhao L, Zheng S, Ma X, et al. Henoch-schönlein purpura with testicular necrosis: Sonographic findings at the onset, during treatment, and at follow-up. Urology. 2017; 107:223-225.
Author Info
Vahid Khajehreza-Shahri1, Sara Gifani2, Paria Dehghanian3, Reza Nazarzadeh4, Ali Mohammad Pourbagher-Shahri5 and Seyed Ali Alamdaran6*2Department of Pediatrics, Mashhad University of Medical Sciences, Mashhad, Iran
3Department of Pediatric Pathology, Mashhad University of Medical Sciences, Mashhad, Iran
4Department of Pediatric Surgery, Mashhad University of Medical Sciences, Mashhad, Iran
5Department of Medicine, Birjand University of Medical Sciences, Birjand, Iran
6Department of Paediatric Radiology, Mashhad University of Medical Sciences, Mashhad, Iran
Received: 23-Aug-2021 Accepted: 06-Sep-2021 Published: 13-Sep-2021, DOI: 10.14534/j-pucr.20212675563
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
