Case Report - (2022) Volume 9, Issue 1
Horseshoe kidney with single ureter system associated with choledochal cyst: A case report
Akshay Baheti*, Apoorva Kulkarni, Shahaji Deshmukh, Dhvani Shah, Abhaya Gupta and Paras KothariAbstract
The horseshoe kidney is the most prevalent renal fusion abnormality. A horseshoe kidney with only one ureter is a rare malformation. Choledochal cyst is cystic dilatation of bile duct. Horseshoe kidney with a single ureter and other associations have been reported in literature, however none of these cases have been associated with choledochal cyst. Surgeons must proceed cautiously when dealing with a Horseshoe kidney patient.
Keywords
Horseshoe kidney, single ureter, choledochal cyst
Introduction
The horseshoe kidney is a developmental defect which often occurs at 4-6 weeks of intrauterine life and is the most prevalent renal fusion abnormality, affecting upto 0.25% of the general population [1]. Horseshoe kidney is usually asymptomatic but association with ureteropelvic junction obstruction, infection, and urolithiasis has been frequently reported and other rare associations including polycystic horseshoe kidney, malignancies, and vascular anomalies have been reported. The incidence of renal pelvis cancer associated with horseshoe kidney has been estimated at 19.8% and renal cell carcinoma has accounted for approximately 50.0% of malignancies found in horseshoe kidney. The incidence of renal cell carcinoma is, however, the same in the population with nonfused kidney. A horseshoe kidney with only one ureter is a rare malformation with unknown etiology. Although horseshoe kidney with a single ureter and other associations has been reported in literature none of these cases had associated choledochal cyst [2]. However, there is a case reported in literature of a horse shoe kidney with Caroli’s disease but with normal ureteric system [3].
Choledochal cyst is congenital cystic dilatation of bile duct, occurring anywhere between liver and duodenum. The choledochal cyst is divided into five different types based on Todani’s classification. The pathogenic mechanism responsible for development of choledochal cysts are poorly understood till date [4].
Association of choledochal cyst along with horseshoe kidney with a single system ureter seems to be first case to be reported in literature to best of our knowledge.
Case Presentation
One month female was admitted with jaundice and fever. Patient had elevated levels of total and direct bilirubin. Patient was antenatally diagnosed case of left hydronephrosis.
On MRCP there was fusiform dilatation of Common hepatic duct, proximal and mid Common bile duct. Common hepatic duct, proximal and mid Common bile duct measures 6 mm, 7.2 mm and 8 mm respectively with abrupt duct cut off and non-visualization of distal intrapancreatic Common bile duct suggestive of choledochal cyst (Fig 1). There is mild to moderate dilatation of central and peripheral intrahepatic biliary radicles with liver parenchymal disease.
Fig 1: Magnetic resonance cholangiopancreatography.
CT Urography was suggestive of horseshoe kidney with lower poles fusion. Left moiety measures 5.2 × 2.8 × 1.9 cm. Right moiety measures 4.8 × 2.3 × 1.7 cm. There was gross dilatation of left pelvicalyceal system with parenchymal thinning of left moiety and minimal excretion from left moiety on delayed scan. Ureters could not be identified. Urinary bladder appeared normal with contrast opacification (Fig 2).
Fig 2: CT Urography.
MCU was done suggestive of normal bladder capacity with no vesoicoureteric reflux.
EC renogram showed decreased left moiety function (28.4%) with ERPF of 15.7 ml/min, delayed cortico- calyceal transit with obstructed excretion. There was preserved right moiety function (71.6%) with ERPF of 39.75 m/min with normal cortico-calyceal transit and non-obstructed excretion in a case of horseshoe kidney.
Treatment
Patient underwent excision of choledochal cyst with hepaticoduodenostomy and cholecystectomy at 1½ month of age.
A month later patient underwent non dismembered Heinicke Mickuliz pyeloplasty for left pelviureteric junction obstruction.
Intraoperative findings were horseshoe kidney with right intrarenal pelvis with right small ureter joining left ureter just distal to narrowed left pelviureteric junction and forming single common ureter draining both moieties of horse shoe kidney. Double j stent removed at six week (Fig 3).
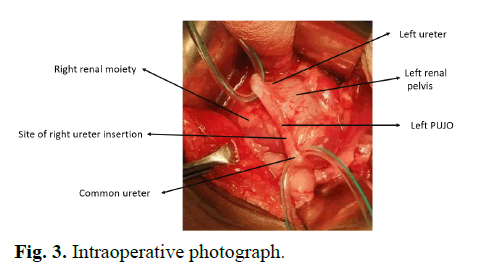
Fig 3: Intraoperative photograph.
Results and Discussion
The most prevalent renal fusion abnormality, the horseshoe kidney occurs as a result of anomalous fusion of lower poles of the kidney at the level of developing inferior mesenteric artery forming a parenchymatous isthmus. Rarely there may be fusion of mid or upper poles. It occurs during the metanephric stage of renal embryogenesis [5,6].
HSK is characterized by three major malfunctions: alterations in vascular supply, rotation and the aberrant position. Horseshoe kidney patients have a higher ureteropelvic junction and their ureters enter pelvis at higher level, that might contribute to an increased prevalence of urinary problems [7].
Horseshoe kidney disease patients are often asymptomatic, but can be associated with abnormalities like pelviureteric junction obstruction, infectious diseases, cancer, urolithiasis, polycystic disease [8].
Multiple ureteric anomalies associated with horseshoe kidney such as unilateral single ectopic ureter, bilateral single-system ectopic ureters, complete unilateral duplication of ureter and pelvicalyceal system and bilateral duplication of the pelvis and ureter .malignant neoplasia in the horseshoe kidney with pyelic fusion and crossed single ureter [9-12].
There are cases of horseshoe kidney single ureteric system and associated anomalies like multiple renal cysts, abdominal aortic aneurysm and neoplasia in horseshoe kidney and crossed single ureter reported in literature [13,14].
Todani, et al. classified choledochal cysts into 5 major subtypes. Type 1 is the most common followed by Type IV A. Type V, is also known as Caroli disease [15]. Right upper quadrant mass, jaundice, and abdominal pain; the classical triad is present more commonly in children. At presentation, approximately 85 percent of children have at least two of the triad traits [16]. Ultrasound is the best initial investigation of choice and MRCP is often the “gold standard” in such cases [17].
Conclusion
Ours is first case reporting association of choledochal cyst with horseshoe kidney and single ureteric system. An HSK patient should be dealt with extreme caution. A meticulous clinical and radiographic evaluation is required since HSK poses a diagnostic and surgical difficulty because of several of related abnormalities.
Conflict of Interest
None declared.
Consent to Publication Statement
Author(s) declared taking informed written consent for the publication of clinical photographs/material (if any used), from the legal guardian of the patient with an understanding that every effort will be made to conceal the identity of the patient, however it cannot be guaranteed.
References
- Cassell A, Jalloh M, Diop PS, et al. A review of rare associations of horseshoe kidney: Highlight of a rare clinical case of polycystic horseshoe kidney, liver cyst, and uterine prolapse. Urol. 2020; 8:22-28.
[CrossRef], [Google Scholar]
- Peres LA, Ferreira JR, Bader SL. Horseshoe kidney with cysts and a single ureter: A case report. J Bras Nefrol. 2010; 32:416-7.
[CrossRef], [Google Scholar] [Pubmed]
- Bodas A, Maluenda C, Rivilla F, et al. Caroli's syndrome and horseshoe kidney: A case report. Acta Paediatr. 2001; 90:469-71.
[CrossRef], [Google Scholar] [Pubmed]
- Machado NO, Chopra PJ, Al-Zadjali A, et al. Choledochal cyst in adults: Etiopathogenesis, presentation, management, and outcome-case series and review. Gastroenterol Res Pract. 2015.
[CrossRef], [Google Scholar]
- Natsis K, Piagkou M, Skotsimara A, et al. Horseshoe kidney: A review of anatomy and pathology. Surg Radiol Anat. 2014; 36:517-26.
[CrossRef], [Google Scholar] [Pubmed]
- Phraim Vikram RKE, Battula SR. Horseshoe kidney: A review article. Int J Res Med Sci 2015; 3:3004-7
- Frego M, Bianchera G, Angriman I, et al. Abdominal aortic aneurysm with coexistent horseshoe kidney. Surg Today. 2007; 37:626-30.
[CrossRef], [Google Scholar] [Pubmed]
- Obidike S, Woha A, Aftab F. Fused ureters in patient with horseshoe kidney and aortic abdominal aneurysm. J Surg Case Rep. 2014; 2014:rju113.
[CrossRef], [Google Scholar]
- Agarwal S, Yadav RN, Kumar M, et al. Horseshoe kidney with unilateral single ectopic ureter. Case Rep. 2018.
[CrossRef], [Google Scholar] [Pubmed]
- Khong PL, Peh WC, Mya GH, et al. Horseshoe kidney with bilateral single system ectopic ureters. Aust N Z J Surg. 1996; 66:773-6.
[CrossRef], [Google Scholar] [Pubmed]
- Tyagi V, Dar TI, Khawaja AR, et al. Horseshoe kidney with complete unilateral duplication of ureter and pelvicalyceal system-a case report. Urol J. 2014; 10:1162-4.
[CrossRef], [Google Scholar] [Pubmed]
- Christoffersen J, Iversen HG. Partial hydronephrosis in a patient with horseshoe kidney and bilateral duplication of the pelvis and ureter. Scand J Urol Nephrol. 1976; 10:91-3.
[CrossRef], [Google Scholar] [Pubmed].
- Ghonge N, Jasuja S. Polycystic horseshoe kidney: Dealing with double trouble. Clin Kidney J. 2014; 7:413.
[CrossRef], [Google Scholar]
- Costa RP, Schaal CH, Navarro FC. Neoplasia in horseshoe kidney with pyelic fusion and crossed single ureter. Int Braz J Urol. 2004; 30:319-20.
- Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977; 134:263-9.
[CrossRef], [Google Scholar] [Pubmed]
- Lipsett PA, Pitt HA, Colombani PM, et al. Choledochal cyst disease: A changing pattern of presentation. Annals of surgery. 1994; 220:644-52.
[CrossRef], [Google Scholar] [Pubmed]
- Mabrut JY, Bozio G, Hubert C, et al. Management of congenital bile duct cysts. Dig Surg. 2010; 27:12-8.
[CrossRef], [Google Scholar] [Pubmed]
Author Info
Akshay Baheti*, Apoorva Kulkarni, Shahaji Deshmukh, Dhvani Shah, Abhaya Gupta and Paras KothariReceived: 14-Feb-2022, Manuscript No. PUCR-22-54386; , Pre QC No. PUCR-22-54386(PQ); Editor assigned: 16-Feb-2022, Pre QC No. PUCR-22-54386(PQ); Reviewed: 28-Feb-2022, QC No. PUCR-22-54386; Revised: 02-Mar-2022, Manuscript No. PUCR-22-54386 (R); Published: 07-Mar-2022, DOI: 10.14534/j-pucr.2022.289
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
