Case Series - (2024) Volume 11, Issue 4
Neonatal imperforate hymen: A case series
Abdelrahman S. Elnour*, Shazali Mohammed Ahmed, Diaaeldin Yassen and Faisal NugudAbstract
Imperforate Hymen (IH) is a rare congenital anomaly of the female genital tract, with an incidence of 0.05%-0.1%, characterized by the complete obstruction of the vaginal opening. While IH is generally isolated anomaly, it can be associated with other genitourinary malformations. IH is often diagnosed during adolescence, neonatal diagnosis is extremely rare, with an incidence of 0.006%. IH diagnosis can be made by inspecting the external genitalia, with abdominal ultrasound aiding in the detection of hydrometrocolpos and urinary tract dilation. Late diagnosis of IH can lead to severe complications such as urinary tract obstruction, hydronephrosis, renal failure, infections, subfertility, and endometriosis. Treatment involves hymenectomy or hymenotomy, allowing effective fluid drainage. Early detection is essential for preventing morbidity. This report presents three cases of neonatal IH, each presenting with abdominal distension and urinary difficulties, one of them complicated with acute kidney injury due to urinary obstruction. Emergency hymenectomy was performed in all cases, resulting in excellent outcomes. This report emphasizes the need for healthcare providers to include IH in the differential diagnosis for female neonates with abdominal mass and urinary issues. Early detection through high index suspicion and thorough genital examinations can prevent complications and improve outcomes.
Keywords
Imperforate hymen, Neonatal diagnosis, Urinary obstruction, Abdominal mass, Hymenectomy
Introduction
Bladder Imperforate Hymen (IH) is a rare congenital anomaly of the female genital tract, characterized by the complete obstruction of the vaginal opening. It has an approximate incidence of 0.05%-0.1% [1]. While IH is usually an isolated anomaly, it can be associated with other malformations in the genitourinary tract such as vaginal or uterine septum, atresia, renal agenesis, duplicated ureter, as well as anorectal and vertebral abnormalities [2].
The vagina develops from the Mullerian ducts and the urogenital sinus. Proliferation of cells at the caudal tip of the fused Mullerian ducts results in a solid vaginal cord. This cord elongates to meet the sinovaginal bulbs, which are endodermal evaginations from the posterior aspect of the urogenital sinus. Cranial extension of the sinovaginal bulbs and their fusion with the lower end of the vaginal cord form a vaginal plate. During embryological development, the vaginal plate usually ruptures, leaving a fold of mucous membrane at the vaginal entrance. Failure of canalization of this tissue will result in an imperforate hymen [2,3].
McKusick-Kaufman syndrome is a rare autosomal recessive syndrome characterized by hydrometrocolpos, polydactyly, and congenital heart defects. Bardet-Biedl syndrome, on the other hand, is a heterogeneous group of autosomal recessive disorders characterized by retinal dystrophy or retinitis pigmentosa, postaxial polydactyly, obesity, nephropathy, and mental disturbances or mental retardation. While both syndromes may present with hydrometrocolpos, they are more commonly associated with vaginal atresia or transverse vaginal septum rather than imperforate hymen [3]. Most cases of IH are diagnosed in post menarche adolescent girls, with the main presentations being amenorrhea, lower abdominal pain, or urinary obstruction. However, the diagnosis of imperforate hymen within the perinatal or neonatal period is extremely rare, with an estimated incidence of 0.006%. Vaginal secretions induced by maternal estrogen may lead to hydrocolpos and hydrometrocolpos, presenting as an abdominal mass in female neonates [1].
The diagnosis of IH can be made by inspection of the external genitalia, in patients who present with a bulging, bluish hymen membrane. Ultrasound of the abdomen and pelvis may accurately depict a pelvic cystic mass as well urinary tract dilatation. Although IH is a benign congenital disorder, late detection and diagnosis may potentially result in severe morbidity. Without the proper management, IH can lead to infections, subfertility, endometriosis, and in rare cases, hydronephrosis and renal failure [4]. The treatment of choice is often a cruciate incision or excision of the hymen. However, for patients desiring virginity, hymen- preserving surgeries like simple vertical incision and annular hymenotomy are considered. Other treatments include the use of a carbon dioxide laser [1].
Case Presentation
Case 1 and 2
Two female neonates, aged five and seven days respectively, were delivered vaginally. Both presented with difficulty in urination and gradually increasing abdominal distension. Upon examination, palpable pelviabdominal masses, a plugging hymen, and compressed ureteral orifices were observed. After admission, urethral stents were inserted. Blood tests showed normal results, while abdominal ultrasound revealed a distended fluid-filled vagina with mild bilateral hydronephrosis. There was no family history of similar problem. Both neonates underwent hymenectomy with a cruciate incision with excision of the central part of the hymen. The output was whitish and milky in case 1 and chocolate-like in case 2 (Figure 1).
Fig. 1. Abdominal ultrasound images of a five-day-old female. a) Neonate showing distended fluid-filled vagina; b) Mild bilateral hydronephrosis; c) The output observed was whitish and milky in case 1, indicating successful relief of hymenal obstruction; d) Pelvic examination of a seven-day-old female neonate demonstrating palpable pelviabdominal masses; e) A plugging hymen; g) Post-operative images following hymenectomy with a cruciate incision.
Case 3
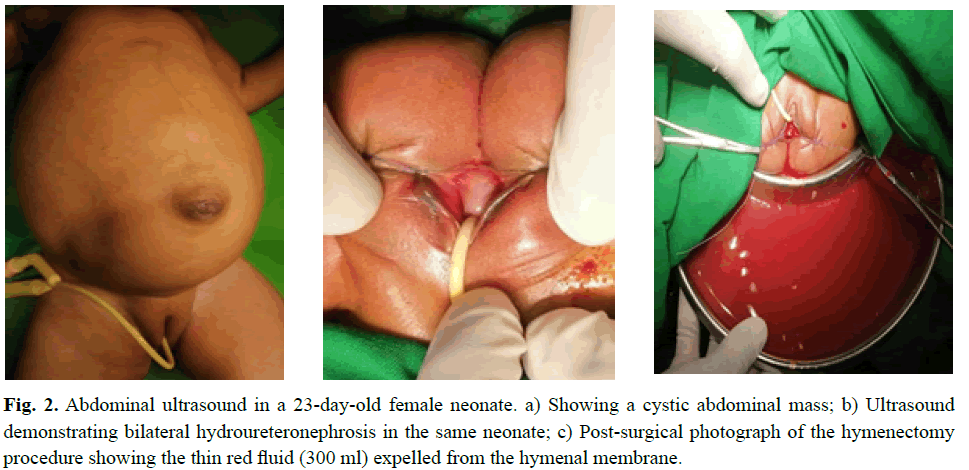
A female neonate, aged 23 days, was delivered vaginally at the hospital. She presented with gradually increasing abdominal distension and straining during urination. Her mother noticed that her diaper had been dry for the last 24 hours. Upon admission to the Pediatric department, she was diagnosed with an abdominal mass and Acute Kidney Injury (AKI). On physical examination she appeared ill and distressed, with lower abdominal distension and a plugging hymeneal membrane. Her blood urea was 238 mmol/l, serum creatinine was 6.5 mmol/l, and serum potassium was 5.3 mmol/l. Ultrasound showed a cystic abdominal mass and bilateral hydroureteronephrosis. After resuscitation, emergency hymenectomy was performed. The output was 300 ml of thin red fluid (Figure 2).
Fig. 2. Abdominal ultrasound in a 23-day-old female neonate. a) Showing a cystic abdominal mass; b) Ultrasound demonstrating bilateral hydroureteronephrosis in the same neonate; c) Post-surgical photograph of the hymenectomy procedure showing the thin red fluid (300 ml) expelled from the hymenal membrane.
The renal impairment and sepsis responded well to treatment. She was discharged after 10 days of admission.
Results and Discussion
Abnormalities of the female reproductive tract are encountered in approximately 2% to 3% of women. Imperforate Hymen (IH) is a rare congenital anomaly in which the hymeneal membrane obstructs the outflow of the female genital tract. It represents the most common congenital cause of genital outflow obstruction in females. Embryologically, failure of canalization of the vaginal plate results in the persistence of an imperforate hymeneal membrane [5].
Although an association with other congenital anomalies has been reported, isolated imperforate hymen is the most common finding. IH remains asymptomatic until puberty [3,4]. Perinatal diagnosis of is uncommon; in a review of 253 patients with IH, only 6.7% had a prenatal diagnosis. Additionally, 69.5% of patients presented at an age older than 12 years, with only 11% being neonates [1]. None of our neonates had a prenatal diagnosis of IH. The diagnosis of IH can be easily made through physical examination alone, eliminating the need for laboratory testing or radiographic evaluations. Observation of the hymen and visualization into the vaginal vault are best accomplished by applying gentle labial traction with the child in the supine frog position, using good light. Delayed diagnosis may lead to obstructive uropathy through compression of the lower urinary tract, resulting in hydroureters, hydronephrosis, and sometimes a life-threatening renal failure, as seen in case three [6,7]. Familial cases of imperforate hymen have been described in literature. McIlroy and Ward described three sisters with imperforate hymen in one family in 1930 [8]. Since then, many familial cases have been documented. However, no familial occurrence was observed in our case series [7,9].
The treatment of IH consists of hymenotomy or hymenectomy, that permits the accumulated fluid to drain. Various types of incisions, such as simple vertical, T-shaped, cruciform, cyclical, and cruciate, have been described [10]. In our case series, we utilized the cruciate incision technique, with trimming of the central part of the hymen membrane. The vaginal mucosa was sutured to the introital edge with interrupted absorbable sutures to prevent stenosis. A urethral stent should be in place before the incision to protect the urethra.
Conclusion
Imperforate hymen is a rare condition that may easily be overlooked without an early diagnosis. Early detection is essential, as the postsurgical prognosis is excellent when detected and treated promptly. Therefore, it’s essential that healthcare providers, especially gynecologists, midwives, and paediatricians, should examine every female patient at birth.
References
- Lee KH, Hong JS, Jung HJ, et al. Imperforate hymen: A comprehensive systematic review. J Clin Med. 2019;8(1):56.
[Crossref] [Google Scholar] [PubMed]
- Khedkar K, Lamture YR, Lohia S, et al. A female infant with rectovestibular fistula and imperforate hymen. J Indian Assoc Pediatr Surg. 2023;28(2):177-178.
[Crossref] [Google Scholar] [PubMed]
- El-Messidi A, Fleming NA. Congenital imperforate hymen and its life-threatening consequences in the neonatal period. J Pediatr Adolesc Gynecol. 2006;19(2):99-103.
[Crossref] [Google Scholar] [PubMed]
- Lardenoije C, Aardenburg R, Mertens H L. Imperforate hymen: a cause of abdominal pain in female adolescents. BMJ Case Rep. 2009;.2008-0722.
[Crossref] [Google Scholar] [PubMed]
- Basaran M, Usal D, Aydemir C. Hymen sparing surgery for imperforate hymen: case reports and review of literature. J Pediatr Adolesc Gynecol. 2009;22(4).
[Crossref] [Google Scholar] [PubMed]
- Posner JC, Spandorfer PR. Early detection of imperforate hymen prevents morbidity from delays in diagnosis. Pediatrics. 2005;115(4):1008-1012.
[Crossref] [Google Scholar] [PubMed]
- Ramphul M, Perry L, Bhatia C. Neonatal imperforate hymen with hydrocolpos. Case Rep. 2016.
[Crossref] [Google Scholar] [PubMed]
- McIlroy DL, Ward IV. Three cases of imperforate hymen occurring in one family. Proc R Soc Med. 1930;23(5):633-634.
[Crossref] [Google Scholar] [PubMed]
- Sakalkale R, Samarakkody U. Familial occurrence of imperforate hymen. J Pediatr Adolesc Gynecol. 2005;18(6):427-429.
[Crossref] [Google Scholar] [PubMed]
- Sorrentino F, Angioni S, Pontis A, et al. Laparoscopically assisted treatment of imperforate hymen in a patient with Ventritrulo-Peritoneal (VP) shunt for congenital hydrocephalous: A case report. Int J Surg Open. 2018;15:66-68.
Author Info
Abdelrahman S. Elnour*, Shazali Mohammed Ahmed, Diaaeldin Yassen and Faisal NugudReceived: 25-Jul-2024, Manuscript No. PUCR-24- 143193; , Pre QC No. PUCR-24- 143193; Editor assigned: 29-Jul-2024, Pre QC No. PUCR-24- 143193; Reviewed: 12-Aug-2024, QC No. PUCR-24- 143193; Revised: 19-Aug-2024, Manuscript No. PUCR-24- 143193; Published: 26-Aug-2024, DOI: 10.14534/j-pucr.20222675660
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.